Americans died of drug overdoses in record numbers as the pandemic spread across the country, federal researchers reported Wednesday, the result of lost access to treatment, rising mental health problems and wider availability of dangerously potent new street drugs.
In the 12-month period that ended in April, more than 100,000 Americans died of overdoses, up almost 30% from the 78,000 deaths in the prior year, according to provisional figures from the National Center for Health Statistics. The figure marks the first time the number of overdose deaths in the United States has exceeded 100,000 a year, more than the toll of car crashes and guns combined. Overdose deaths have more than doubled since 2015.
Administration officials said Wednesday they will expand access to medications like naloxone, which can reverse an opioid overdose, by encouraging states to pass laws that will make it more widely available and promoting its use by Americans.
“I believe that no one should die of an overdose simply because they didn’t have access to naloxone,” said Dr. Rahul Gupta, director of National Drug Control Policy. “Sadly, today that is happening across the country, and access to naloxone often depends a great deal on where you live.”
Although recent figures through September suggest the overdose death rate may have slowed, the grim tally signals a public health crisis whose magnitude was both obscured by the Covid pandemic and accelerated by it, experts said.
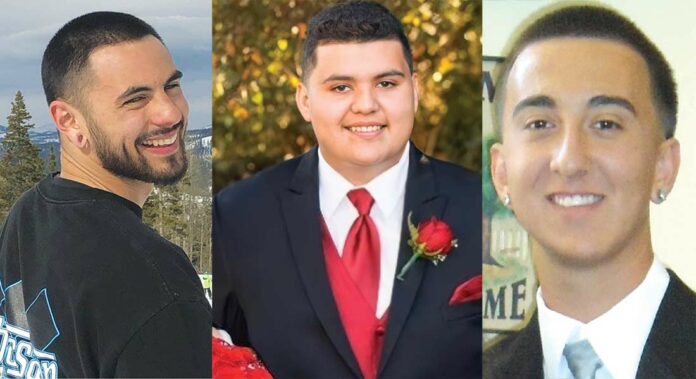
In Santa Clara County, overdose deaths—specifically from the powerful opioid fentanyl—rose from 27 in 2019 to 88 in 2020, according to authorities. This year, the county is on track to record more than 100 drug overdose deaths before Dec. 31. The crisis has prompted local families to try to raise awareness of the dangers of street drugs any way they can.
“These are numbers we have never seen before,” said Dr. Nora Volkow, director of the National Institute on Drug Abuse.
The fatalities have wide repercussions, since most of them occur among people ages 25-55, in the prime of life, she added.
“They leave behind friends, family and children, if they have children, so there are a lot of downstream consequences,” Volkow said. “This is a major challenge to our society.”
The rise in deaths—the vast majority caused by synthetic opioids—was fueled by widespread use of fentanyl, a fast-acting drug that is 100 times as powerful as morphine. Increasingly, fentanyl is added surreptitiously to other illegally manufactured drugs to enhance their potency.
Overdose deaths related to use of stimulants like methamphetamine, cocaine, and natural and semi-synthetic opioids, such as prescription pain medication, also increased during the 12-month period.
Fentanyl’s ubiquity and the unique social conditions caused by the pandemic have combined to create a perfect storm, experts said. While some drug users seek out fentanyl, Volkow said, others “may not have wanted to take it. But that is what is being sold, and the risk of overdose is very high.”
“Many people are dying without knowing what they are ingesting,” she said.
People struggling with addiction and those in recovery are prone to relapse, Volkow noted. The initial pandemic lockdowns and subsequent fraying of social networks, along with the rise in mental health disorders like anxiety and depression, helped create a health maelstrom.
So, too, did the postponement of treatment for substance abuse disorders, as health care providers nationwide struggled to tend to huge numbers of coronavirus patients and postponed other services.
Dr. Joseph Lee, president and CEO of the Hazelden Betty Ford Foundation, said community and social support that was lost during the pandemic, along with the closing of schools, contributed to rising overdose deaths.
“We’re seeing a lot of people who delayed getting help, and who seem to be more sick,” Lee said.
The vast majority of these deaths, about 70%, were among men ages 25-54. And while the opioid crisis has been characterized as one primarily impacting white Americans, a growing number of Black Americans have been affected as well.
There were regional variations in the death counts, with the largest year-over-year increases—exceeding 50%—in California, Tennessee, Louisiana, Mississippi, West Virginia and Kentucky. Vermont’s toll was small but increased 85% during the reporting period.
Increases of about 40% or greater were seen in Washington state, Oregon, Nevada, Colorado, Minnesota, Alaska, Nebraska, Virginia and the Carolinas. Deaths dropped in New Hampshire, New Jersey and South Dakota.
“If we had talked a year ago, I would have told you, ‘Deaths are skyrocketing.’ But I would not have guessed it would get to this,” said Dr. Andrew Kolodny, medical director of the Opioid Policy Research Collaborative at Brandeis University’s Heller School for Social Policy and Management.
Most of those who died probably already suffered from addiction, or were in recovery and relapsed, an ever-present risk exacerbated during times of stress and isolation, Kolodny said. And many of those with an addiction to synthetic opioids very likely became addicted after being given prescription opioids by medical providers.
“Teenagers are routinely being given opioids to this day when their wisdom teeth come out,” he said.
President Joe Biden’s American Rescue Plan Act includes $1.5 billion for the prevention and treatment of substance use disorders, and $30 million to fund local services for people struggling with addiction, including syringe exchange programs.
Federal funds can also be used now to buy rapid fentanyl test strips that people can use to check whether drugs have been laced with fentanyl.
But critics say the response has been inadequate given the magnitude of the public health emergency. They have called for new funding streams to provide universal access to treatment, and for treatment centers in every county that offer same-day access to substance abuse treatment.
For example, physicians still need federal permission to prescribe buprenorphine, a first-line treatment for opioid use disorder, which limits the number of providers.
“If you really want to see deaths come down, you have to make it much easier for someone who is addicted to opioids to access treatment, particularly with buprenorphine,” Kolodny said. “It has to be easier to get treatment than to buy a bag of dope.”